World Antibiotic Awareness Week
Theme: Antimicrobials: handle with care
World Antimicrobial Awareness Week (WAAW) aims to increase awareness of global antimicrobial resistance (AMR) and to encourage best practices among the general public, health workers and policy makers to avoid the further emergence and spread of drug-resistant infections.
As resistance grows to a wider range of drugs, we have broadened the focus of this campaign from antibiotics to all antimicrobials.
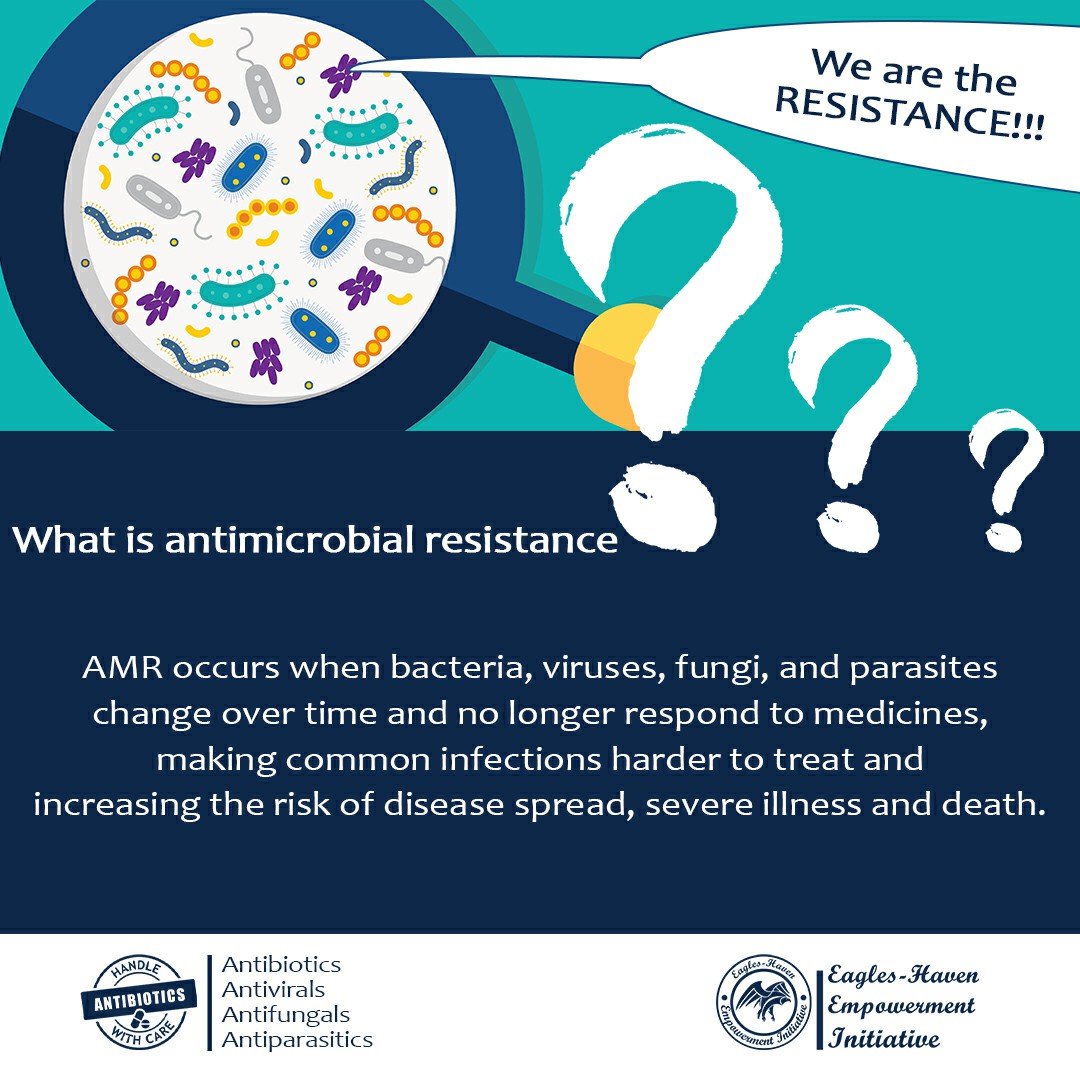
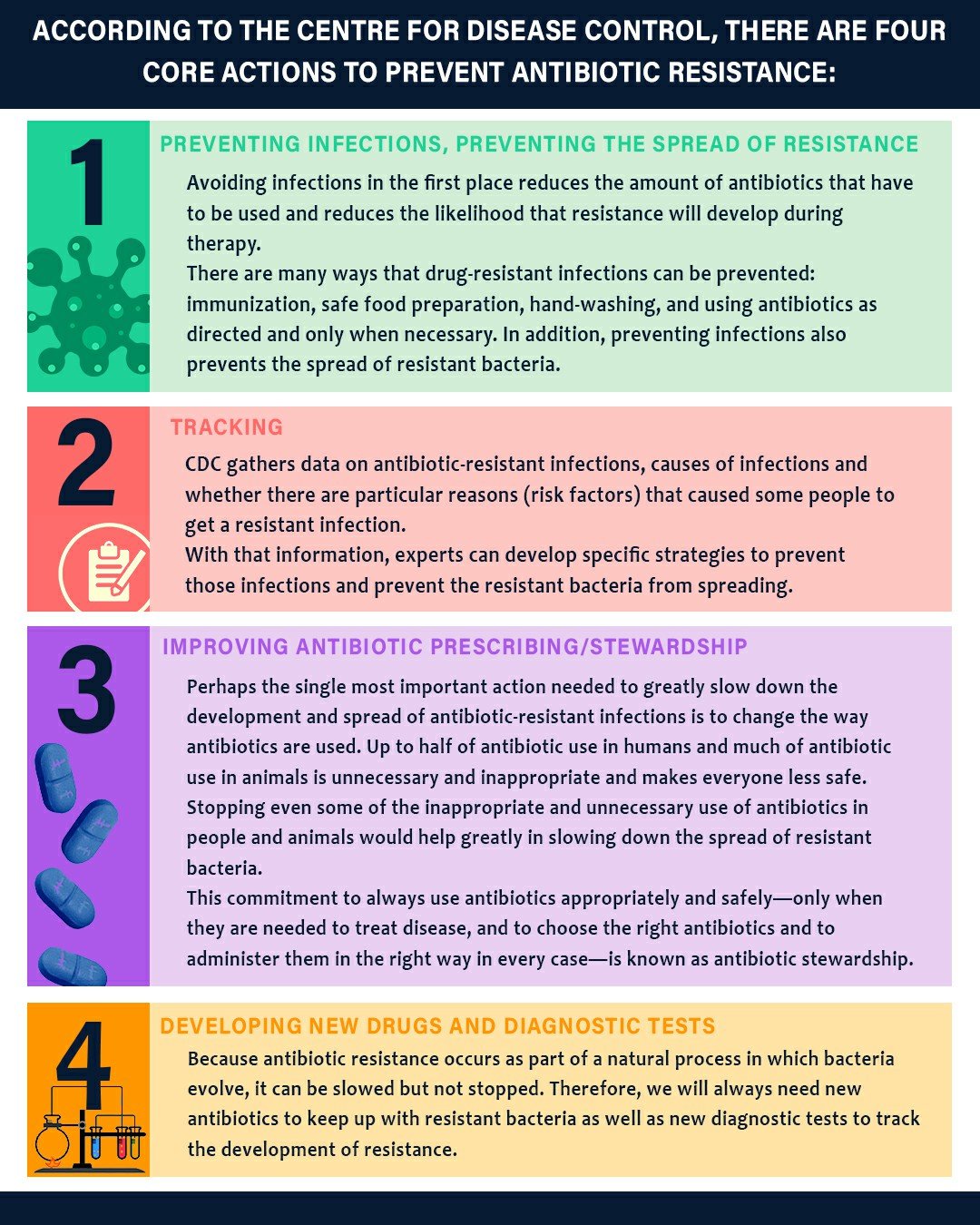
What is antimicrobial resistance?
AMR occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines, making common infections harder to treat and increasing the risk of disease spread, severe illness and death.
Many factors have accelerated the threat of AMR worldwide—including overuse and misuse of medicines in humans, livestock and agriculture, as well as poor access to clean water, sanitation and hygiene.
Why is AMR increasing?
-Misuse and overuse of antimicrobials in humans, animals and plants
-Lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals
-COVID-19
Key facts
Antimicrobial resistance (AMR) is a global health and development threat. It requires urgent multisectoral action in order to achieve the Sustainable Development Goals (SDGs).
WHO has declared that AMR is one of the top 10 global public health threats facing humanity.
Misuse and overuse of antimicrobials are the main drivers in the development of drug-resistant pathogens.
Lack of clean water and sanitation and inadequate infection prevention and control promotes the spread of microbes, some of which can be resistant to antimicrobial treatment.
The cost of AMR to the economy is significant. In addition to death and disability, prolonged illness results in longer hospital stays, the need for more expensive medicines and financial challenges for those impacted.
Without effective antimicrobials, the success of modern medicine in treating infections, including during major surgery and cancer chemotherapy, would be at increased risk.
What accelerates the emergence and spread of antimicrobial resistance?
AMR occurs naturally over time, usually through genetic changes. Antimicrobial resistant organisms are found in people, animals, food, plants and the environment (in water, soil and air). They can spread from person to person or between people and animals, including from food of animal origin.
The main drivers of antimicrobial resistance include the misuse and overuse of antimicrobials; lack of access to clean water,sanitation and hygiene (WASH) for both humans and animals; poor infection and disease prevention and control in health-care facilities and farms; poor access to quality, affordable medicines, vaccines and diagnostics; lack of awareness and knowledge; and lack of enforcement of legislation.
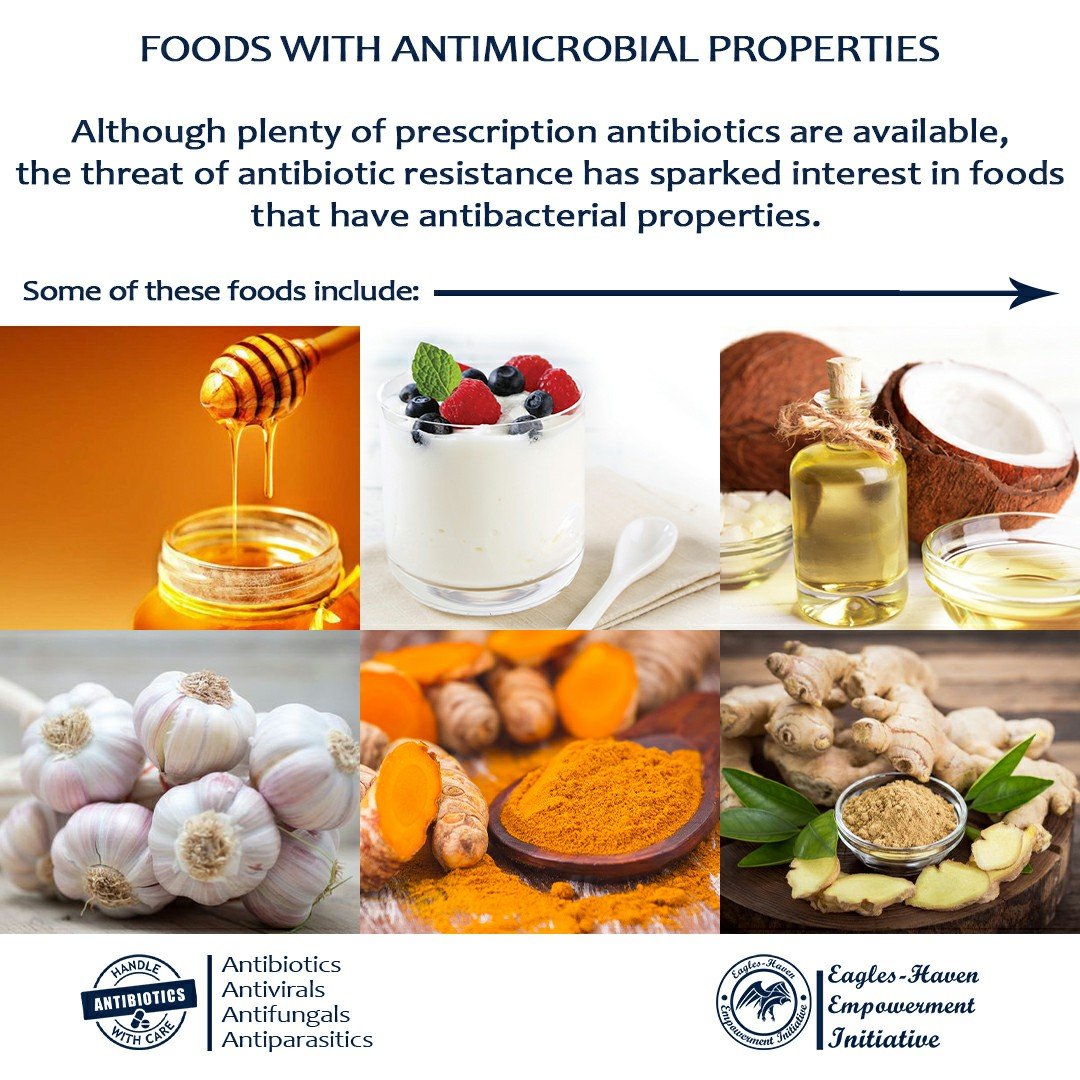
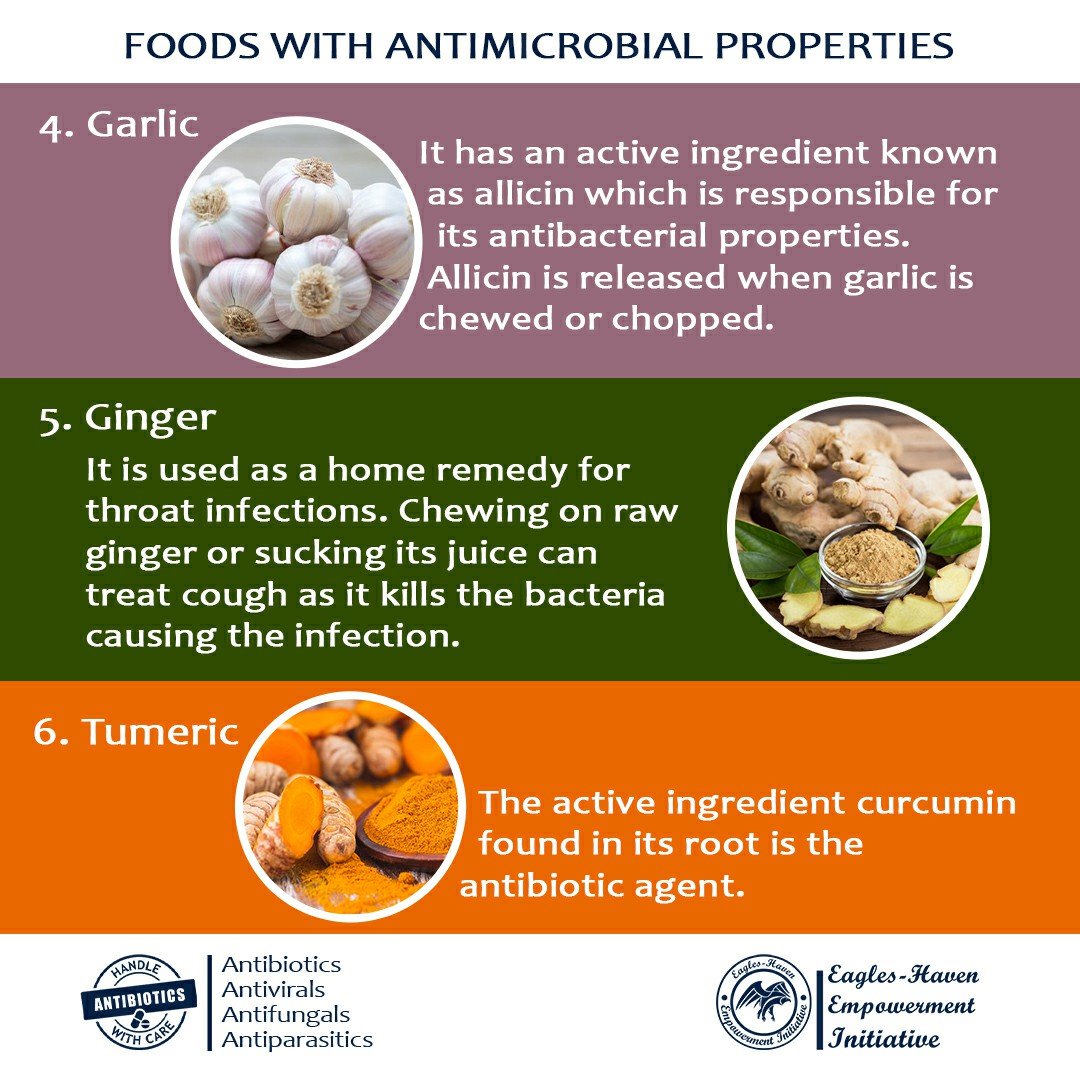
Foods with antimicrobial properties
Although plenty of prescription antibiotics are available, the threat of antibiotic resistance has sparked interest in foods that have antibacterial properties.
(SEE BLOG FOR MORE DETAILS!)
Economic impact of antimicrobial resistance
One reason antimicrobial-drug resistance has recently become a concern is its economic impact. The Institute of Medicine estimates the annual cost of infections caused by antibiotic-resistant bacteria to be U.S.$4 to $5 billion.
For the physicians, the main economic problems that resistance presents are related to ineffective treatment. There are likely to be multiple antimicrobial agents which are effective in curing a given infection but with rising antimicrobial resistance, these agents diminish in number. Therefore, the economic impact of diminishing effectiveness of a given drug or group of drugs depends on the availability of other drugs.
Economic impact is also measured in terms of consequences arising from illness and death, specifically the added cost of treatment of a resistant organism, since patients pay retail prices for drugs and services. Such charges are assumed directly when patients pay their own bills or absorbed indirectly when added costs of multiple drugs and services result in increasing premiums for patients who have health-care coverage.
Antimicrobial drugs represent a way to provide cost-effective care to patients who are part of a defined population being served. The economic cost of antimicrobial-drug resistance for health-care businesses is in the measures they must take to preserve the effectiveness of antimicrobial agents in the care group. These measures may include costs for a series of different drugs and services, as well as for personnel time, supplies, space, and equipment for institutional programs to deal with antimicrobial-drug resistance (e.g., pharmacy and therapeutics committees,antimicrobial-drug use review, practice guidelines).
Since antimicrobial drugs enhance both prevention and treatment of infections, society considers them a valuable resource. As resistance diminishes this resource, a societal goal would be to minimize resistance and therefore the forces that produce resistance.
In the jargon of economics, antimicrobial agents are a scarce resource, that is, one in which consumption (current use) decreases its effectiveness (future value). Any use of antimicrobial agents enhances the likelihood of resistance. From a societal viewpoint, then, appropriate use of antimicrobial drugs for treatment and prevention of infection would lead to an appropriate or acceptable decrease in the value of antimicrobial effectiveness. Conversely, overuse or misuse of antimicrobial drugs would create an inappropriate decrease in these resources. When treating one person leads to decreased effectiveness in treating the next person receiving the drug, society is affected adversely.